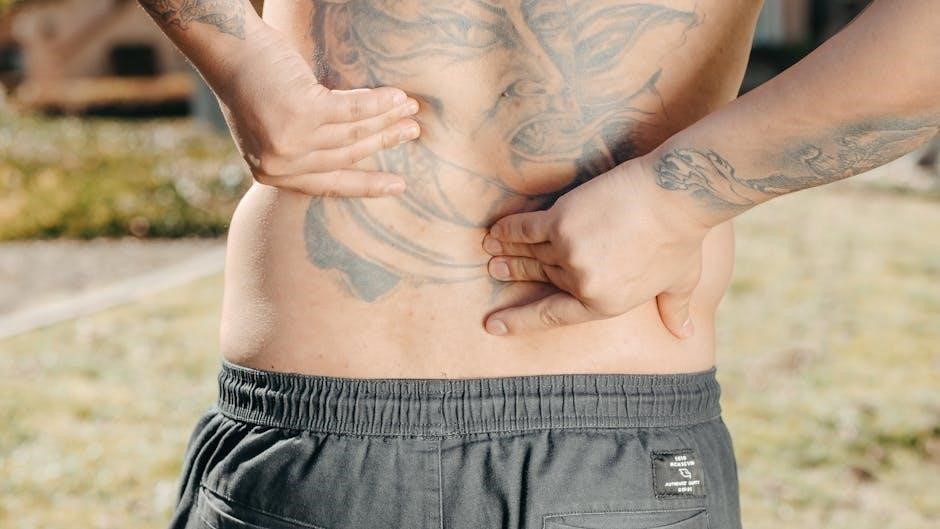
Low back pain is a common condition affecting millions worldwide, often disrupting daily activities and reducing quality of life. Special tests play a crucial role in diagnosing underlying causes, ensuring accurate assessment and effective treatment plans. Understanding its prevalence and impact is essential for developing a comprehensive management strategy.
Prevalence and Impact of Low Back Pain
Low back pain is one of the most prevalent musculoskeletal conditions worldwide, affecting approximately 84% of adults at some point in their lives. It is the second most common complaint presented to healthcare providers, significantly impacting quality of life and productivity. The economic burden is substantial, with estimated annual costs exceeding $100 billion in the U.S. alone. Chronic low back pain can lead to mental health challenges, such as stress and anxiety, further complicating recovery. Despite its widespread nature, most cases are self-limiting, resolving within weeks without advanced interventions. However, persistent or severe pain necessitates thorough evaluation, including special tests, to identify underlying causes and guide effective treatment. Early assessment is critical to preventing long-term disability and improving patient outcomes.
Importance of Special Tests in Diagnosis
Special tests are essential in diagnosing low back pain, enabling clinicians to identify specific pathologies and rule out serious conditions. These tests, such as the Straight Leg Raise Test (SLR) and Slump Test, help assess nerve root compression, disc herniation, and joint instability. By isolating specific movements and structures, they provide insights into the underlying causes of pain, guiding targeted treatment. Early and accurate diagnosis is critical to prevent chronicity and improve outcomes. Special tests also help differentiate between mechanical and non-mechanical pain, ensuring appropriate referrals and interventions. While imaging and other diagnostic tools are valuable, special tests often suffice for initial assessment, reducing the need for costly procedures. Their role in clinical decision-making underscores their importance in effective patient care and management. Regular use of these tests by clinicians ensures comprehensive evaluation and tailored treatment plans for low back pain.
Overview of Diagnostic Approaches
The diagnosis of low back pain involves a systematic approach to identify the underlying cause and guide appropriate treatment. Initially, a thorough patient history and physical examination are conducted to gather information about symptoms, onset, and contributing factors. Special tests, such as the Straight Leg Raise Test (SLR) and Slump Test, are employed to assess nerve root compression and disc-related issues. Imaging studies like X-rays, MRIs, and CT scans are reserved for cases with red flags or persistent pain despite conservative management. Electrophysiological tests, such as EMG, may also be used to evaluate nerve function. A biopsychosocial assessment is often incorporated to address psychological and social factors influencing pain. The combination of clinical evaluation, special tests, and advanced imaging ensures a comprehensive diagnostic strategy, enabling clinicians to develop tailored treatment plans for patients with low back pain.
Clinical Evaluation of Low Back Pain
Clinical evaluation involves a thorough patient history, physical examination, and posture assessment to identify underlying causes of low back pain. It guides diagnostic and management strategies effectively.
Patient History and Symptom Assessment
A detailed patient history is critical in evaluating low back pain, focusing on the onset, nature, and progression of symptoms. Key factors include the location, intensity, and duration of pain, as well as aggravating or relieving factors. The OPQRST mnemonic (Onset, Palliation/Provocation, Quality, Region, Severity, Timing) helps structure the assessment. Patients should be asked about medical history, prior injuries, and lifestyle factors. Red flags, such as fever, weight loss, or neurological symptoms, are noted to identify serious conditions. A thorough symptom assessment guides further diagnostic steps and treatment planning. Understanding the patient’s functional limitations and psychosocial factors, like stress or anxiety, is also essential for a holistic approach. This process ensures tailored management and improves outcomes for individuals with low back pain.
Physical Examination Techniques
The physical examination for low back pain begins with inspection, evaluating posture and spinal alignment. The clinician observes for abnormalities such as scoliosis or a flattened lumbar lordosis. Palpation is used to identify areas of tenderness, muscle spasms, or tightness. Range of motion tests assess flexibility and mobility, noting limitations or pain during movements like flexion, extension, or rotation; Special tests, such as the Straight Leg Raise or Slump Test, are performed to detect nerve root irritation or disc herniation. Strength and reflex testing are also conducted to evaluate neurological function. These techniques, combined with patient history, help pinpoint the underlying cause of pain, guiding appropriate diagnostic imaging or further evaluation. A systematic approach ensures a thorough and accurate assessment, which is vital for effective treatment planning.
Red Flags for Serious Conditions
Red flags in low back pain indicate potentially serious underlying conditions that require immediate attention. These include recent trauma, unexplained weight loss, bladder or bowel dysfunction, fever, or severe neurological deficits like foot drop or cauda equina syndrome. Patients with a history of cancer, osteoporosis, or prolonged corticosteroid use are at higher risk. Symptoms such as progressive numbness, weakness, or loss of reflexes also warrant urgent investigation. The presence of these flags necessitates advanced imaging or specialist referral to rule out conditions like fractures, infections, or spinal malignancies. Early identification of red flags ensures timely intervention, preventing complications and improving outcomes; Clinicians must remain vigilant for these signs during patient assessment to provide appropriate care.

Special Tests for Low Back Pain
Special tests for low back pain, such as the SLR and slump test, help identify specific conditions like disc herniation or nerve root compression. These assessments guide targeted treatment plans.
Straight Leg Raise Test (SLR)
The Straight Leg Raise Test (SLR) is a widely used clinical assessment for identifying nerve root irritation, particularly in cases of suspected lumbar disc herniation. During the test, the patient lies supine while the examiner passively flexes the hip to 90 degrees with the knee held straight. A positive result is indicated by radiating pain below the knee, typically between 30° and 70° of hip flexion. The sensitivity of the SLR varies depending on the patient’s condition but is particularly useful for diagnosing nerve root compression. It is often performed bilaterally to compare symptoms and assess the severity of nerve involvement. The SLR is a cornerstone in the physical examination of low back pain, providing valuable insights for clinicians to guide further diagnostic and therapeutic interventions.
Slump Test
The Slump Test is a neurological examination used to assess nerve tension and mobility, particularly in the lumbar spine and lower extremities. It is commonly utilized to evaluate patients with sciatic pain or suspected nerve root compression. During the test, the patient sits with their legs extended and then slumps forward, allowing their head and neck to flex naturally. The examiner then applies gentle pressure to the patient’s shoulders to further flex the thoracic and lumbar spine. Pain or discomfort radiating down the leg during this maneuver may indicate nerve root irritation or disc herniation. The Slump Test is valued for its ability to replicate symptoms and guide diagnostic and therapeutic decisions. While its sensitivity varies, it remains a reliable tool in the clinical assessment of low back pain when combined with other evaluations.
Crossed Straight Leg Raise Test
The Crossed Straight Leg Raise Test (XSLR) is a specialized physical examination used to diagnose lumbar disc herniation, particularly at the L4-L5 or L5-S1 levels. The test involves the patient lying supine while the examiner lifts the unaffected leg to 70-90 degrees. If this movement causes pain in the affected leg, it may indicate nerve root compression. The crossed component refers to pain radiating to the opposite leg, which is highly specific for disc herniation. The test is particularly useful when the Straight Leg Raise Test (SLR) is negative but clinical suspicion of nerve root involvement remains. A positive result is strongly correlated with imaging findings of disc herniation. The XSLR is a valuable tool in the clinical arsenal for identifying patients who may benefit from surgical intervention or further diagnostic imaging.

Diagnostic Imaging for Low Back Pain
Imaging techniques like X-rays, MRIs, and CT scans help identify structural issues, such as herniated discs or fractures, guiding accurate diagnoses and treatment plans for low back pain.
Role of X-rays in Diagnosis
X-rays are commonly used to evaluate low back pain, particularly when suspecting fractures, spinal misalignment, or degenerative changes. They provide clear images of bony structures, helping to rule out serious conditions like vertebral fractures or spondylolisthesis. However, X-rays are limited in assessing soft tissues, such as discs or nerves, making them less effective for diagnosing issues like herniated discs or spinal stenosis. Despite this, X-rays remain a valuable initial diagnostic tool, especially for acute pain or when trauma is involved. They are often recommended for patients with red flags, such as recent injury or prolonged pain, to guide further investigation or treatment. Clinicians may combine X-ray findings with clinical history and physical examination to determine the need for advanced imaging like MRI or CT scans.
MRI Scans for Soft Tissue Assessment
MRI scans are highly effective for assessing soft tissue abnormalities in low back pain cases, such as herniated discs, nerve root compression, and spinal stenosis. Unlike X-rays, MRIs provide detailed images of soft tissues, including the spinal cord, discs, and ligaments. This makes them particularly useful for diagnosing conditions that involve nerve compression or inflammation. MRI scans are non-invasive and do not involve radiation, making them a safer option for long-term use. They are often recommended when conservative treatments fail to resolve symptoms or when red flags, such as numbness or weakness, are present. While MRI scans are valuable, they should be used judiciously to avoid unnecessary costs and radiation exposure. Clinicians typically reserve MRI scans for cases where surgical intervention may be required or when the cause of pain remains unclear after other evaluations;
CT Scans for Detailed Imaging
CT scans provide high-resolution imaging of the lumbar spine, making them particularly useful for assessing bony structures, such as vertebral fractures, spondylolisthesis, or spinal deformities. They are often used when MRI is contraindicated or unavailable. CT scans are effective for identifying structural abnormalities, such as disc herniations or facet joint osteoarthritis, and can help guide injections or surgical interventions. While MRIs are superior for soft tissue evaluation, CT scans offer excellent detail for bony pathology. They are commonly recommended for patients with a history of trauma or suspected fractures. However, CT scans involve radiation exposure, so they are typically reserved for cases where the benefits outweigh the risks. Clinicians often use CT scans to confirm diagnoses when other imaging modalities are inconclusive, ensuring precise treatment planning for chronic or acute low back pain cases.

Physical Examination Techniques
Physical examination techniques are essential for assessing low back pain, involving posture evaluation, palpation, and movement tests to identify structural issues or muscle imbalances guiding treatment plans effectively.
Inspection and Postural Assessment
Inspection and postural assessment are critical components of evaluating low back pain. The examiner begins by observing the patient’s stance, noting any visible asymmetries, such as uneven shoulder or hip alignment. The natural spinal curvatures, including lordosis (inward curvature of the lower back) and kyphosis (outward curvature of the upper back), are evaluated. A loss of lumbar lordosis, often seen as a flat lower back, may indicate muscle imbalances or structural issues. The patient is assessed from both anterior and posterior views to identify any deviations from normal posture. This visual examination provides valuable clues about potential underlying causes of pain, such as muscle spasms, vertebral misalignment, or soft tissue strain. Palpation may follow to confirm tenderness or tightness in specific areas, aiding in the diagnosis and guiding further testing or treatment.
Palpation for Tender Points
Palpation is a fundamental technique in physical examination to identify tender points in patients with low back pain. Using the fingertips, the examiner applies gentle pressure to assess muscle tension, joint mobility, and soft tissue tenderness. This helps differentiate between muscle-related pain and joint-related pain. Tender points may indicate localized inflammation, muscle spasms, or trigger points. The examiner typically palpates key areas, including the lumbar paraspinal muscles, sacroiliac joints, and gluteal muscles. Noting the location and intensity of tenderness provides insights into potential underlying conditions, such as facet joint syndrome or sacroiliac dysfunction. Palpation also helps guide further diagnostic steps or therapeutic interventions, making it a vital tool in the clinical assessment of low back pain.
Range of Motion and Flexibility Tests
Range of motion (ROM) and flexibility tests are essential components of the physical examination for low back pain. These assessments evaluate the ability to perform movements such as flexion, extension, lateral bending, and rotation. Limitations in ROM or the presence of pain during these movements can indicate underlying issues like muscle imbalances, joint dysfunction, or structural damage. The examiner observes the patient’s ability to perform these movements actively and passively, noting any restrictions or discomfort. Flexibility tests, such as the hamstring stretch, can identify tightness that may contribute to low back pain. These tests help differentiate between mechanical and non-mechanical causes of pain, guiding further diagnostic steps or treatment. Accurate ROM and flexibility assessments are crucial for developing personalized rehabilitation plans to restore mobility and reduce discomfort.
Management and Rehabilitation Strategies
Effective management of low back pain combines conservative approaches, physical therapy, and patient education. Early intervention and tailored rehabilitation strategies enhance recovery, reducing pain and improving functionality.
Conservative Management Approaches
Conservative management is often the first line of treatment for low back pain, focusing on non-invasive methods to alleviate symptoms and promote recovery. This approach typically includes physical therapy, exercise programs, and lifestyle modifications. Physical therapy involves tailored exercises to improve flexibility, strength, and posture, reducing strain on the lower back. Heat or ice therapy may be recommended to relieve discomfort and inflammation. Additionally, patient education plays a crucial role, emphasizing proper lifting techniques and ergonomic adjustments to prevent recurrence. Medications, such as over-the-counter pain relievers, are often used to manage pain and inflammation. Activity modification, including avoiding heavy lifting or prolonged sitting, is also encouraged. Conservative methods are effective for most patients, with many experiencing significant improvement within a few weeks. Early intervention and adherence to these strategies can help restore function and reduce the risk of chronic pain.
Role of Physical Therapy
Physical therapy is a cornerstone in the management of low back pain, offering a personalized approach to restore function and reduce discomfort. Trained therapists design programs that include strengthening exercises, stretching, and posture correction to address muscle imbalances and improve mobility. Techniques such as manual therapy, soft tissue mobilization, and core stabilization are commonly used to alleviate pain and enhance stability. Physical therapy also emphasizes education, teaching patients proper lifting techniques, ergonomic adjustments, and exercises for long-term pain prevention. By addressing both physical and psychological factors, physical therapy empowers patients to take an active role in their recovery, promoting independence and reducing the likelihood of recurrence. This non-invasive approach is widely recommended as a first-line treatment for low back pain, often leading to significant improvements in both symptoms and quality of life.
Surgical Interventions for Chronic Pain
Surgical interventions are typically reserved for cases of chronic low back pain where conservative treatments have failed to provide relief. Procedures such as spinal fusion, discectomy, or laminectomy are considered when pain is caused by structural issues like herniated discs, spinal stenosis, or spondylolisthesis. Surgery aims to relieve nerve compression, stabilize the spine, or correct mechanical abnormalities. Patient selection is critical, with factors like the severity of symptoms, imaging findings, and overall health influencing the decision. While surgery can offer significant pain relief for appropriate candidates, it is not a guarantee and carries risks such as infection, bleeding, or complications from anesthesia. A multidisciplinary approach, including input from orthopedic surgeons, neurologists, and pain specialists, is essential to determine if surgery is the best option for chronic low back pain.

Psychological and Social Factors
Psychological factors like stress and anxiety can significantly influence low back pain perception and recovery. Social influences, such as work-related stress, also play a role in exacerbating symptoms and impacting overall well-being.
Impact of Stress and Anxiety
Stress and anxiety can significantly exacerbate low back pain by increasing muscle tension and altering pain perception. Chronic stress often heightens sensitivity to pain, making it more challenging to manage. Additionally, anxiety can amplify the emotional burden of pain, creating a cycle that worsens symptoms. Addressing psychological factors is crucial, as they can delay recovery and reduce the effectiveness of physical treatments. Relaxation techniques, such as deep breathing and mindfulness, can help mitigate stress and anxiety, thereby alleviating pain. Understanding the interplay between mental health and physical discomfort is essential for developing a holistic treatment plan. By incorporating stress management strategies, individuals can better cope with low back pain and improve their overall well-being.
Role of Pain Management Programs
Pain management programs play a vital role in addressing chronic low back pain by adopting a multidisciplinary approach. These programs combine medical, psychological, and physical therapies to help individuals cope with pain effectively. They often include relaxation techniques, exercise routines, and education on pain management strategies. The goal is to reduce reliance on medication and empower patients to take control of their condition. Such programs also address underlying stress and anxiety, which are common contributors to chronic pain. By fostering a supportive environment, pain management programs enable patients to improve their quality of life and return to normal activities. They are particularly beneficial for those with complex or persistent pain, offering a comprehensive approach to recovery and well-being.
Importance of Patient Education
Patient education is a cornerstone in managing low back pain, empowering individuals to understand their condition and actively participate in recovery. Educating patients about proper posture, safe lifting techniques, and appropriate exercises can significantly reduce pain flare-ups and improve functionality. It also helps in setting realistic expectations and promoting adherence to treatment plans. By addressing misconceptions and fostering a positive mindset, patient education enhances overall well-being. Additionally, it equips individuals with strategies to manage stress and anxiety, which often exacerbate chronic pain. Continuous education enables patients to take control of their recovery, reducing reliance on medication and minimizing the risk of recurrence. Ultimately, patient education is key to achieving long-term pain relief and improving quality of life.

Advanced Diagnostic Tools
Advanced diagnostic tools like EMG assess nerve function, while bone scans detect traumatic injuries. These tools, combined with a biopsychosocial assessment, provide a comprehensive understanding of low back pain.
Electrophysiological Tests (EMG)
Electrophysiological tests, such as electromyography (EMG), are crucial for assessing nerve and muscle function in patients with low back pain. EMG measures the electrical activity of muscles, helping diagnose conditions like nerve root compression or damage. This test is particularly useful when symptoms suggest nerve involvement, such as radiating pain or numbness. By identifying abnormal muscle activity, EMG can pinpoint the exact nerve affected, guiding targeted treatment. It is often complemented by nerve conduction studies to provide a comprehensive evaluation. EMG is minimally invasive and provides valuable insights into the neurological aspects of low back pain, making it an essential tool in advanced diagnostic protocols.
Bone Scans for Traumatic Injuries
Bone scans are advanced imaging techniques used to evaluate traumatic injuries in patients with low back pain. They are particularly useful for detecting fractures, infections, or tumors that may not be visible on X-rays. By using small amounts of radioactive material, bone scans highlight areas of increased bone activity, indicating potential damage or disease. This test is especially valuable when there is a history of trauma or suspicion of a stress fracture. Bone scans provide critical information for diagnosing and managing conditions that require immediate attention, ensuring appropriate treatment and preventing further complications. They are often recommended when other imaging methods are inconclusive, offering a detailed view of bone health in the lower back region.
Biopsychosocial Assessment
A biopsychosocial assessment is a comprehensive evaluation that considers the interplay of biological, psychological, and social factors in low back pain. This approach recognizes that pain is not solely a physical phenomenon but is influenced by emotional state, stress levels, and environmental conditions. The assessment includes tools to identify non-organic signs, such as superficial tenderness or non-anatomic pain, which may indicate psychological components. It also evaluates the impact of stress, anxiety, and depression on pain perception. Social factors, like job satisfaction and family support, are examined to understand their role in pain chronicity. This holistic approach helps clinician